Diabetes Task Force
Diabetes Task Force Solutions (“DTFS”) is a team of professional healthcare providers, health administrators, and patients with considerable business expertise, to ensure that our solutions are evidence based, comprehensive, cost effective, and sustainable. DTFS has worked with a number of organizations to develop unique; evidence based comprehensive diabetes prevention and management programs ranging from education to community-based prevention and management models, and to state-of-the-art virtual diabetes center.Our philosophy is based on empowerment and motivation of patients to play a leading role in managing their chronic diseases through culturally sensitive and holistic self-education interactive education programs; providing healthcare professionals with innovative technology based tools for better treatment and monitoring of patients; and integrated solutions for healthcare services to cost effectively manage their resources while providing efficient services to the clients.
Services
- Evaluation of diabetes management program effectiveness
- Designing and implementing diabetes prevention and management programs and strategies
- Developing clinical outcome measures
- Developing digital health solutions

|
| Care Models |

|
| Digital Health |
|
| Virtual Care |
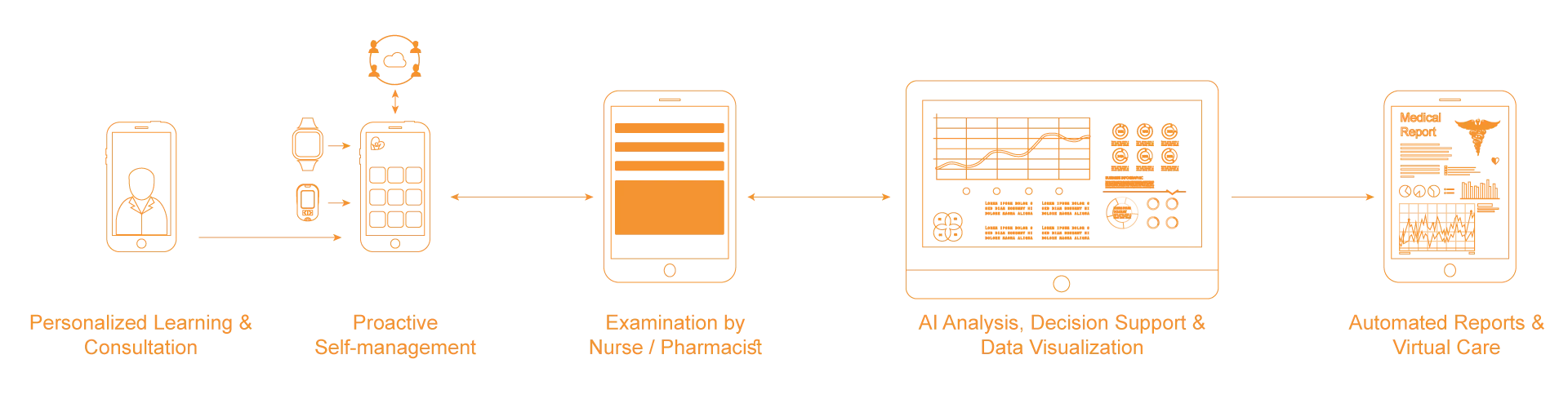
Our Diabetes Proactive Management Ecosystem
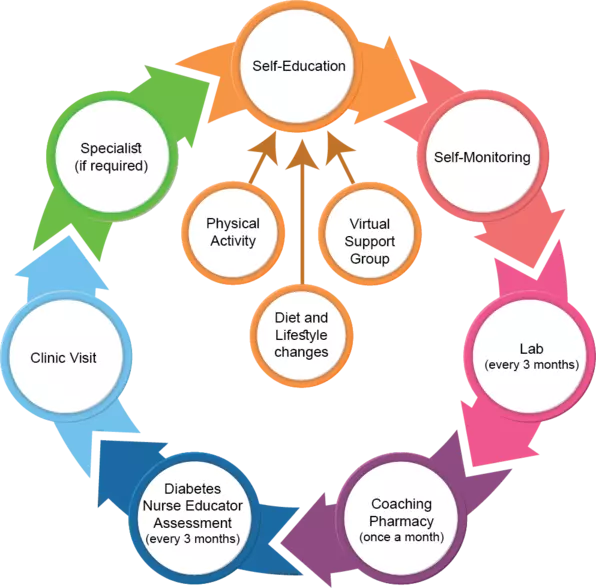
Diabetes is a progressive disease, requiring a proactive, patient-focused care approach to prevent health complications that negatively impact patients and healthcare systems. Our Diabetes Management Ecosystem addresses gaps in the current delivery of chronic-diseases care. This includes an imbalance between the number of patients with diabetes and the number of healthcare providers in addition to a necessary enhancement of the overall efficiency of diabetes-care workflow and health outcomes.
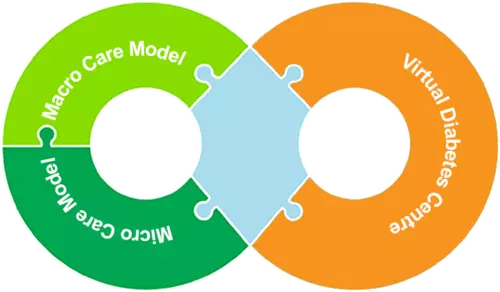
DTFS’ Diabetes Management Ecosystem is based on the empowerment of Patients and Healthcare Providers by combining the latest information technology with evidence-based health care practices into a holistic proactive care system. It consists of Macro/Micro diabetes care models and our proprietary digital health solution, the Virtual Diabetes Center. The ecosystem is customizable to meet the requirement of different health care system and available resources.
DTFS’ Diabetes Management Ecosystem is based on the empowerment of Patients and Healthcare Providers by combining the latest information technology with evidence-based health care practices into a holistic proactive care system. It consists of Macro/Micro diabetes care models and our proprietary digital health solution, the Virtual Diabetes Center. The ecosystem is customizable to meet the requirement of different health care system and available resources.
Our Digital Health Solutions
The VIrtual Diabetes Center ("VDC") is a proprietary digital health ecosystem for diabetes and other chronic diseases management; it facilitates the collaboration between healthcare providers, and Integrates patients’ self-management and lifestyle data with current health conditions and historical medical records. Utilizing proprietary automated algorithms, VDC organizes and provides such information in easy-to-review visuals, giving healthcare team members a comprehensive understanding of the relation between patients’ lifestyle, their diabetes management, and the current prescribed treatment, all which is essential for successful management of chronic diseases and improved health outcomes.
VDC consists of four separate Cloud-based applications. Each function as an independent application or as an integrated solution to provide complete diabetes-care solution based on your requirements. These are Diabetes Case Management, Patients Health Management, Patient Diabetes Self-Education and Continuing Medical Education.
VDC consists of four separate Cloud-based applications. Each function as an independent application or as an integrated solution to provide complete diabetes-care solution based on your requirements. These are Diabetes Case Management, Patients Health Management, Patient Diabetes Self-Education and Continuing Medical Education.
VDC
Patient Education Portal
Cloud based interactive multimedia technology can be used to augment current diabetes education methods. A number of research studies have demonstrated the effectiveness of interactive multimedia diabetes education tools as an initial education following diagnoses and as continuous education for patients and their families. VDC Patient Education Portal provides patients with in-depth knowledge about type 2 diabetes and how to manage it. Following the diagnoses by family physician, patients are advised to start learning about diabetes through the Virtual Diabetes Learning Center prior to attending educational classes at the Diabetes Education Classes; this will help to motivate the patients to manage their diabetes. Delay in receiving proper education could lead to denial which is the most common barrier to diabetes self-management.
Personal Health Records
Successful management of diabetes requires continuous monitoring of multiple health indicators and lifestyle parameters such as blood sugar levels, blood pressure, physical activity, and diet by patients with the supervision of diabetes healthcare providers. The Virtual Diabetes Center’s Patient Health Record Management “MyVDC” is a user friendly, on-line health data recording and data visualization tool. MyVDC organizes and tracks the patient’s home test results, and presents the data using easy to understand visuals, and associated educational materials empowering the patient to understand how their lifestyle and treatment impacts their diabetes. Through a secured link to the Virtual Diabetes Center’s Diabetes Case Management program, healthcare teams have access to patient data for review during clinic visits and for continuous monitoring.
Diabetes Case Management
VDC's Diabetes Case Management ("DCM") is an Electronic Diabetes Visit Records based on diabetes care practical guidelines. Patient registration includes: patient demographics, diabetes history, medical history, family medical history, and cumulative profile. Detailed user friendly forms are used to capture detailed, patient-specific clinical information in a format easily reviewed by clinicians. This information includes: medication, monitoring and hypoglycemia, diet and exercise, cardiac and other complication, life style, physical exam, lab results, and vision. DCM gathers complete flow sheet data and historical medical data and facilitates sharing of recommendations between care team members. Members can use the program to produce comprehensive recommendation letters, letters to patients, and file existing forms which can easily be viewed by the entire team. The reports section of DCM includes a series of standardized reports and customizable queries for outcome analysis.
Diabetes Home Care
DHC developed to support diabetes care for seniors living at retirement and long-term care facilities or receiving home care nursing services. This user-friendly application can be used by patients and/or with the support of Home Care Nurse; monitoring data can also be transferred directly from Bluetooth enabled devices. The application also provides Diabetes Nurse Educators with visuals and analytics to provide patients with optimal diabetes management and continuous monitoring. The application generates comprehensive medical reports for review by family physician and specialists facilitating the integration of diabetes home care with the health care system. Click here for more information
Continuing Medical Education
Diabetes treatment, medications, and guidelines are constantly changing. Our customizable system provides your organization with a tool that keeps your team up to date on the latest changes in the diabetes treatment field. The Virtual Diabetes Center's learning, content, and events management system (LCEMS) provides a multi-user environment where developers, authors, instructional designers, and subject matter experts may create, store, reuse, manage, and deliver digital educational technology content. It also provides the administration, documentation, tracking, reporting and delivery of electronic educational technology (e-learning) courses or training programs. The Virtual Diabetes Center's LCEMS provides secured instant chat room and message board for exchanging knowledge and discussions among registered users. It also has a blog and news feeder managed by the LCEMS administrator to provide registered users with the latest news in the field of diabetes management and research.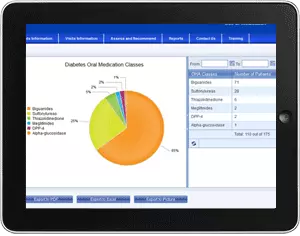
Analytics and Decision Support
VDC generates comprehensive medical reports, decision support based on clinical guidelines, and risk analysis for type 2 diabetes, CKD, and CVD. VDC’s provide comprehensive analytics tools, a series of standardized reports and customizable queries for outcome analysis. Healthcare professionals and administrators can quickly and easily generate statistics regarding patients’ clinic, medications and laboratory results, and treatment outcome using similarity analysis. These statistics and reports can be converted to PDFs and exported into Excel for integration into medical papers or for other uses. The program can also develop a recall list. Patients who have high indicators can receive automated notifications to see their healthcare team.Our Diabetes Care Models
Proactive Care Model
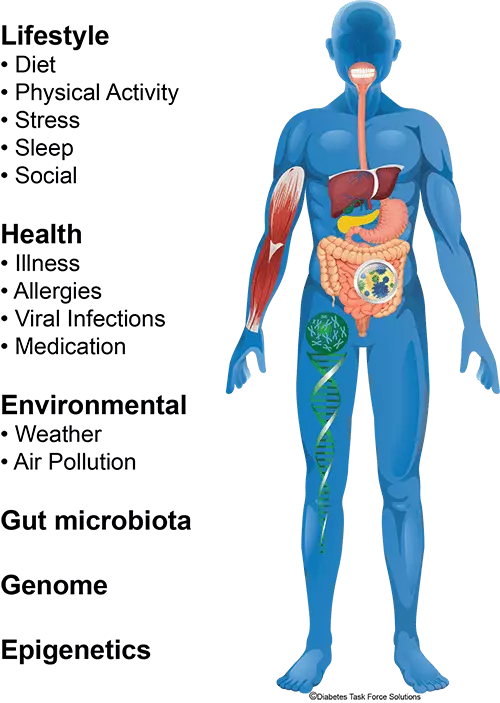
In many parts of the world today, the diabetes care model is based on the acute care model. In the majority of cases, the prescribed treatment for blood sugar control is based on one lab result called A1c. If a patient’s blood sugar is higher than the recommended guidelines, the usual solution is to increase the intake of insulin or other oral medication. This may have serious negative side effects that impact a patient’s quality of life if the medication is wrong or administered incorrectly.
Our proactive approach starts with knowledgeable and motivated patients who are active partners in managing their diabetes, rather than being passive recipients of care. Diabetes is complex and there are many factors that could affect blood sugar control. Also, patients’ genetic makeup affects the effectiveness and potentially adverse impact of diabetes medications.
Diabetes self-management data: diet, physical activity, sleep, stress, allergies, social activities and environmental factors are essential to understanding what affects a patient’s blood sugar levels. Such data are also indicators of preventive actions. Regular monitoring, as well as access to multidisciplinary healthcare providers, is also key to early intervention.
Our proactive approach starts with knowledgeable and motivated patients who are active partners in managing their diabetes, rather than being passive recipients of care. Diabetes is complex and there are many factors that could affect blood sugar control. Also, patients’ genetic makeup affects the effectiveness and potentially adverse impact of diabetes medications.
Diabetes self-management data: diet, physical activity, sleep, stress, allergies, social activities and environmental factors are essential to understanding what affects a patient’s blood sugar levels. Such data are also indicators of preventive actions. Regular monitoring, as well as access to multidisciplinary healthcare providers, is also key to early intervention.
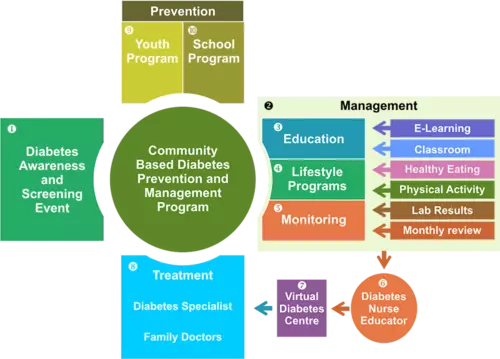
Macro Care Model
Community Based Diabetes Prevention and Management Model A culturally appropriate and holistic model to achieve evidence based outcomes for the prevention and management type 2 of diabetes; a patient focused approach, was developed by DTFS in association with a team of healthcare professionals specialized in diabetes prevention and management, and considerable input from patients and other stakeholders. The model was implemented at a number of First Nations in British Columbia, and has achieved significant results in terms of prevention and management of diabetes and the sustainability and ownership of the disease within the community.
The model consists of six integrated components: Awareness and Motivation, Education, Management and Monitoring, Treatment, Prevention, and Diabetes Management Software. Diabetes Nurse Educators play an integral part in the implementation of the program as the main point of contact for monitoring patients and coordinating treatment activities. This provides intimate motivational access to healthcare which permits alternative and cost-effective approaches to all aspects of diabetes management.
The model consists of six integrated components: Awareness and Motivation, Education, Management and Monitoring, Treatment, Prevention, and Diabetes Management Software. Diabetes Nurse Educators play an integral part in the implementation of the program as the main point of contact for monitoring patients and coordinating treatment activities. This provides intimate motivational access to healthcare which permits alternative and cost-effective approaches to all aspects of diabetes management.
Virtual Care Model
Currently, two mobile diabetes clinics in British Columbia are utilizing the Virtual Diabetes Center's Diabetes Case Management to serve more than 150 remote communities. Each clinic has two trained diabetes nurse educators and an eye technician, the team members travel to the communities and record the health history, complete an examination of patients, and their recommendations. In addition, a full laboratory Point-of-Care testing is completed, as recommended by the Canadian Diabetes Guidelines, and multiple field retinal photographs are taken. This information is virtually accessed by consultants in Endocrinology and Ophthalmology. As a result, complete recommendations for changes in therapy are provided “on line,” via a secure system to the primary care physicians.
Micro Care Model
The model applies our Proactive Care Model, it integrates the expertise of all care team members as an integrated network which includes general practitioners, diabetes nurse educators, specialists, dietitians, pharmacists, social workers, and physical activity trainers. It will also involve local community centres, diabetes education centre, pharmacies, food stores, and other resources that could provide patient support. The model will utilize the Virtual Diabetes Center to link team members, patient self-management, education, and training to maximize the utilization of the advancement in information technology and wearables.
1
Patient Education
Following a diagnosis by a family physician (or through community screening programs), patients are advised to start learning about diabetes. This can be done through an authenticated on-line program prior to attending educational classes at Diabetes Education Centres if available.
This is key to engage patients and their families and to reduce fear and denial.
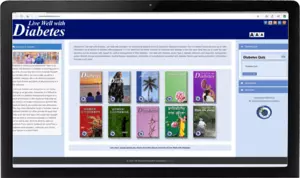
It is recommended that the healthcare provider have his or her own learning program. The Virtual Diabetes Center’s Patient Education Portal has a Learning Content Management System. It is currently used by the British Columbia Endocrine Research Foundation (BCERF) for its Live Well with Diabetes initiative. This program provides culturally sensitive education in nine languages.

2
Diabetes Self-management
Patients must be encouraged by their healthcare provider to monitor and record their blood sugar levels and lifestyle factors to understand how to manage their diabetes. Also, physicians must ask the patient for these data. This information is vital to train the patient on managing diabetes, and recommend lifestyle changes (with the support of other care team including registered dietitians, social workers, physical trainers, etc.), as well as for physicians to prescribe accurate treatment.
Patients can record self-management data manually or use wearable and eHealth tools. All new glucose meters have simple software applications. Unfortunately, a very small percentage of patients and physicians are utilizing them. Patients have to be aware of the large numbers of diabetes applications that collect data for the purpose of marketing. Some applications have not been tested for outcome analysis.
Patients can record self-management data manually or use wearable and eHealth tools. All new glucose meters have simple software applications. Unfortunately, a very small percentage of patients and physicians are utilizing them. Patients have to be aware of the large numbers of diabetes applications that collect data for the purpose of marketing. Some applications have not been tested for outcome analysis.
The patient must be an active participant in their diabetes management.

The Virtual Diabetes Center’s Patient Self-management tool, “MyVDC,” is a user-friendly, on-line, health data-recording tool. This program organizes and tracks the patient’s home test results for the healthcare team to review. The patient is provided with access to educational materials on diabetes to learn how to manage their disease. The program is easy to use and is accessible by personal computers, tablets and smart phones.
Through a secured link to the Virtual Diabetes Center’s Diabetes Case Management program, healthcare teams have access to patient data for review during clinic visits and for continuous monitoring. As well, MyVDC has a notification system alerting the healthcare team if there are any major changes in the blood sugar levels between the clinic visits.
Through a secured link to the Virtual Diabetes Center’s Diabetes Case Management program, healthcare teams have access to patient data for review during clinic visits and for continuous monitoring. As well, MyVDC has a notification system alerting the healthcare team if there are any major changes in the blood sugar levels between the clinic visits.
3
Group Learning
Patients may also attend diabetes education classes at Diabetes Education Centres (if available) or through pharmacies and other not-for-profit organizations to reinforce their knowledge about diabetes management. The patients who begin attending these classes without prior diabetes knowledge are often in a state of fear and denial, as well as are often unable to understand and retain this information.

4
Supporting Lifestyle Changes
Making lifestyle changes and dealing with diabetes are challenging tasks if support isn’t available from healthcare providers or community and online resources. Recreation centres are valuable resources to assist patient with physical activity through group classes and personal trainers. Some of these programs are subsidized by government or not-for-profit organizations.
Encourage patients to seek support from community resources and diabetes associations.
Some supermarkets offer nutritional and health-shopping tours as well as healthy cooking classes. Pharmacies can also provide diabetes education and patient support. Local and virtual diabetes support groups facilitate organizing group activities and educational classes, sometimes with the support of diabetes associations.

5
Motivational Interviewing
Prior to the doctor’s visit and following a group education session, a one-on-one motivational interview with a diabetes nurse educator or a pharmacist with a diabetes education certificate will allow a patient to address specific concerns and review self-management records.
Motivated, knowledgeable and engaged patients manage their diabetes better than passive ones.

The nurse or pharmacist will use a diabetes medical records system to record a patient’s current health conditions, family history and other health complications. The Virtual Diabetes Center’s Diabetes Case Management (DCM) is an electronic diabetes visit record based on diabetes care practice guidelines. User-friendly forms capture detailed, patient-specific clinical information acquired by health care staff that is produced in a format easily reviewed by clinicians. This information includes: patient demographics, diabetes history, medical history, family medical history, medication, monitoring and hypoglycemia, diet and physical activity, cardiovascular and other complications, life style, physical exam, lab results and eye exams.
There are a number of studies that have demonstrated that the active participation of diabetes nurse educators (in some countries they are called diabetes nurse specialists) improves outcomes and reduces costs.
There are a number of studies that have demonstrated that the active participation of diabetes nurse educators (in some countries they are called diabetes nurse specialists) improves outcomes and reduces costs.

6
Clinic Visit
The Virtual Diabetes Center's Diabetes Case Management data visualization allows medical professionals to access and review information on a patient’s current medical status, historical medical data as well as patients’ self-management data.
Data visualization maximizes time utilization during clinic visits and ultimately allows for more precise diagnoses and successful treatment outcomes. Understanding the relation between the patient’s lifestyle and blood sugar control allows physicians to treat the cause rather than the symptoms. This could include circumstances where a patient is dealing with a temporary stressful situation. Therefore, increasing or changing diabetes medication may not be the appropriate treatment.
Data visualization maximizes time utilization during clinic visits and ultimately allows for more precise diagnoses and successful treatment outcomes. Understanding the relation between the patient’s lifestyle and blood sugar control allows physicians to treat the cause rather than the symptoms. This could include circumstances where a patient is dealing with a temporary stressful situation. Therefore, increasing or changing diabetes medication may not be the appropriate treatment.
Using one system and storing data on a clinic’s server overcomes interoperability challenges.

DCM facilitates the coordination among the integrated medical care team and patient self-management to provide better patient care and improve work-flow and productivity of the healthcare system. Members can use the program to automatically produce comprehensive recommendation letters and letters to patients while storing existing forms that can easily be viewed by the entire team. This sharing of information improves efficiency, prevents duplication and provides a more comprehensive view of a patient's condition.
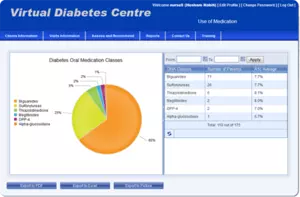
The analytics section of DCM includes a series of standardized reports and customizable queries for outcome analysis. From the database, the healthcare team quickly and easily generates statistics relating to patients’ clinic visits, medications and laboratory results. These statistics and reports can be converted to PDFs and exported into Excel for integration into medical papers or for other uses. The program can also be used to develop a recall list. Patients who have high indicators can receive automated notifications to see their healthcare team.
Eduction and Motivation
In association with BC Endocrine Research Foundation, DTFS have developed a comprehensive multicultural diabetes education program, it is available as a web-based program and in DVD format. Live Well with Diabetes addresses the culture aspects that motivates people to manage their health in Cantonese, Mandarin, Punjabi, Farsi, Arabic, English, French, and Spanish.
The purpose of “Live Well with Diabetes” is to provide a combination of diabetes knowledge and self-management skills as well as heightened self-awareness regarding health, beliefs, needs, and goals. Individuals with diabetes can use this knowledge to make informed decisions about their behavior and act for their self-care. Family and friends can also gain understanding thereby providing a solid support network for the individual with diabetes.
In addition to the development of the application, DTFS has assisted in fundraising activities, conducting pilot project to evaluate the effectiveness of the program, and in the promotion of the program through several conferences and workshops. DTFS has also produced all promotional materials and newsletters. The program was developed in 2005 and updated annually by DTFS, it is accessed by people from many countries and is used by support groups and health organizations.
The purpose of “Live Well with Diabetes” is to provide a combination of diabetes knowledge and self-management skills as well as heightened self-awareness regarding health, beliefs, needs, and goals. Individuals with diabetes can use this knowledge to make informed decisions about their behavior and act for their self-care. Family and friends can also gain understanding thereby providing a solid support network for the individual with diabetes.
In addition to the development of the application, DTFS has assisted in fundraising activities, conducting pilot project to evaluate the effectiveness of the program, and in the promotion of the program through several conferences and workshops. DTFS has also produced all promotional materials and newsletters. The program was developed in 2005 and updated annually by DTFS, it is accessed by people from many countries and is used by support groups and health organizations.

Indigenous Health
Our team has extensive experience working with Indigenous communities developing and implementing culturally appropriate evidence-based diabetes prevention and management initiatives, these include our community-based diabetes prevention and management model “Diabetes and My Nation”, and Diabetes Awareness and Screening Events. We also bring all stakeholders from government agencies, not-for-profit organization, and industries to support these initiatives and build bridges and trust among all participants.
Our Methodology
- Patient focused approach
- Evidence based outcome
- Development of Best Practices
- Participation of all stakeholders during the planning, funding, and implementation stages of the project to ensure the solutions are cost effective, evidence-based, and sustainable
- Management by objective approach
- Maximize the use of information technology when applicable
- Develop implementation procedures for future duplication of the project
- Apply medical ethical protocols
- Protection of patients’ information and ownership of data
- Apply system encryption and data security

Working together to improve diabetes care
Contact us